Alice Chang, Ph.D. works as a Professor of Biochemistry and Molecular Biology with a background in pharmacology, cancer biology, cell biology, biochemistry, and genetics. In the following article, Dr. Alice Chang discusses research findings regarding the intricate molecular mechanisms underlying bladder and prostate cancers, focusing on the complex role of lineage plasticity and the transcription factor FOXA1 in tumor development and progression.
The FOXA (Forkhead Box A) protein family, encompassing FOXA1, 2, and 3, acts as master pioneer transcription factors pivotal for regulating tissue-specific gene expression by facilitating chromatin structure relaxation and enabling the binding of other transcription factors. Bladder cancer, a prevalent malignancy affecting thousands in the United States annually, is characterized by its heterogeneity, with tumors often exhibiting diverse histological features.
Bladder cancer often presents with heterogeneous morphologies, posing challenges in treatment due to their intratumoral genomic and immunologic variability. Specifically, researchers have observed that bladder cancers frequently contain regions of urothelial carcinoma alongside areas showing squamous differentiation. Alice Chang, Ph.D. mentions that this phenomenon is known as lineage plasticity.
Unveiling the Biological Basis and Clinical Implications of Bladder Cancer Heterogeneity
In a bid to elucidate the biological basis and clinical implications of this heterogeneity, scientists conducted integrated genomic analyses of mixed histology bladder cancers. The study revealed that squamous differentiation serves as a marker of genomic and immunologic heterogeneity within bladder cancer tumors and is associated with intrinsic resistance to immunotherapy. Phylogenetic analysis further confirmed that both urothelial and squamous regions within these tumors originate from a common precursor.
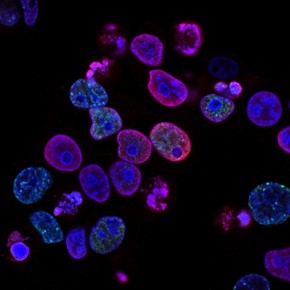
Alice Chang, Ph.D. at the Institute of Biochemistry, CMU notes that despite the marked genomic heterogeneity observed between the co-existent urothelial and squamous differentiated regions, no specific and recurrent genomic alterations were identified. Instead, lineage plasticity in bladder cancers with squamous differentiation was found to be linked to the loss of expression of key transcription factors FOXA1, GATA3, and PPARG, which are critical for maintaining urothelial cell identity. This loss of expression, particularly of FOXA1, was found to activate an interferon signature in squamous cells, influencing their interaction with the immune system.
Moreover, tumors displaying mixed histology were found to be less responsive to immune checkpoint inhibitors targeting PD-L1, a protein crucial for immune therapy efficacy. Dr. Alice Chang implies that the study underscores the importance of understanding the molecular drivers of tumor heterogeneity in devising effective therapeutic strategies for bladder cancer patients.
Investigating the Role of FOXA1 in Prostate Cancer Progression and Treatment Resistance
Furthermore, in the realm of prostate cancer, the role of FOXA1 has also garnered significant attention. Prostate cancer ranks as the second-leading cause of cancer-related mortality among men in the United States. While treatments such as radiation and hormone therapy have shown efficacy in early-stage disease, many patients eventually develop resistance and progress to metastatic castration-resistant prostate cancer (CRPC).
The Pivotal Role of FOXA Proteins in Prostate Cancer Progression and Gene Regulation
In prostate cancer, FOXA1 serves as a critical pioneer factor for the androgen receptor (AR), and the FOXA1-AR signaling pathway is integral to the caner development. Dr. Alice Chang points to the fact that while FOXA1 expression diminishes in neuroendocrine prostate cancer, FOXA2 expression escalates, studies suggest differing roles for these FOXA family members, underscoring the context-specific functions of FOXA proteins in prostate cancer progression.
FOXA1 Downregulation and Its Role in Prostate Cancer Metastasis and Hypoxic Programming
Alice Chang, Ph.D. indicates that recent research has implicated FOXA1 downregulation in prostate cancer metastasis, suggesting its potential tumor-suppressive role in CRPC. To delve deeper into the molecular mechanisms underlying CRPC progression, researchers investigated the impact of FOXA1 downregulation on hypoxic programming within the prostate tumor microenvironment. Through in vitro analyses of prostate cancer cell lines, they discovered that FOXA1 binds to HIF1A, inhibiting its expression. HIF1A, in turn, regulates hypoxia gene expression induced by FOXA1 loss. Furthermore, FOXA1 downregulation was found to promote the infiltration of macrophages into the tumor microenvironment, fostering an immunosuppressive milieu and enhancing cancer cell invasion.
 The Impact of Macrophage Infiltration and Immune Response Modulation in Prostate Cancer
The Impact of Macrophage Infiltration and Immune Response Modulation in Prostate Cancer
Alice Chang, Ph.D. mentions that the infiltration of macrophages into the tumor microenvironment has significant implications for immune response modulation. When macrophages are recruited to the tumor, they can antagonize T-cell function and impair immune responses, exacerbating tumor progression. The findings underscore FOXA1’s pivotal role in regulating hypoxic tumor microenvironments in CRPC and its contribution to prostate cancer progression. Dr. Alice Chang indicates that considering these findings, the researchers caution against therapeutic targeting of FOXA1, as it may lead to lineage plasticity, hypoxia, and CRPC progression. Instead, they advocate for targeting epithelial-mesenchymal transition and hypoxia programs induced by FOXA1 loss as potential strategies to prevent or treat CRPC.
The Future of Targeted Therapies in Bladder and Prostate Cancer
Alice Chang, Ph.D., highlights the complex interplay between transcription factor dysregulation, tumor heterogeneity, and immune modulation in bladder and prostate cancers. Her research underscores the importance of transcription factors like FOXA1 in maintaining cellular identity and regulating the tumor microenvironment. The loss of FOXA1 in bladder cancer leads to significant genomic and immunologic heterogeneity, posing challenges for effective immunotherapy. Similarly, in prostate cancer, FOXA1 downregulation is linked to hypoxic programming and macrophage infiltration, which can exacerbate tumor progression and immune suppression.
These findings emphasize the need for a nuanced approach in developing therapeutic strategies. Rather than directly targeting FOXA1, which could lead to adverse effects such as lineage plasticity and enhanced hypoxia, future therapies should focus on the pathways and mechanisms activated by the loss of FOXA1. By targeting epithelial-mesenchymal transition and hypoxia programs, researchers hope to develop more effective treatments for castration-resistant prostate cancer (CRPC) and other challenging cancer forms.
The research calls for a deeper understanding of the molecular drivers behind tumor heterogeneity and immune modulation. This knowledge is pivotal for devising personalized and precise therapeutic interventions that can improve patient outcomes. As we move forward, the integration of genomic analyses and a comprehensive understanding of transcription factor dynamics will be essential in tackling the complexities of cancer biology. The ultimate goal remains to transform these scientific insights into actionable treatments, providing hope and improved quality of life for cancer patients worldwide.